An operation performed to prevent or limit abnormal motion in the spine by fusing two or more vertebrae. A spinal fusion may be performed as treatment for lower back pain due to "wear and tear" or for numerous other reasons including infection, tumours or broken bones as well as in deformity of the spine such as in scoliosis. The actual fusion (joining together) is done by surgically applying bone graft and/or spinal instrumentation to the level to be fused. A decompressive procedure, such as a laminectomy, may also be performed if required. Any problematic protruding disc material as well as arthritic areas of the spine may also be addressed at the same time.
Generally spinal fusion surgery for back pain is reserved for patients with very specific and disabling pain. Few patients with back pain are considered likely to benefit from the surgery, and for those considered appropriate the likelihood of improvement in the pain following the surgery is around 70%. It should also be remembered that it may take many months for the pain to improve even if the surgery is successful. This relates to the long healing process which follows the surgery. This long period of recovery may be in large part due to slow muscle recovery after surgery.
The bone graft used for a spinal fusion may be autograft (bone taken from your own body) or allograft (bone from a bone bank). As the harvesting of bone (usually from the hip) may be painful, alternatives to using the patient's own bone are being sought very enthusiastically. Some alternative methods include artificially produced bone substitutes and bone forming proteins and electronic implants which generate an electric current around the bone graft and encourage its growth and maturation.
It is generally held that success of a fusion operation is improved by holding the bones in the desired position with screws and rods. There are many different types available although all are similar and there is very little to favour one type over another. If metal is used, it cannot be felt through the skin, mostly does not need to be removed and will not set off the metal detectors at airports!
There are several different ways in which vertebrae may be fused together and the particular technique depends largely of the characteristics of each individual case.
Anterior/Posterior Fusion
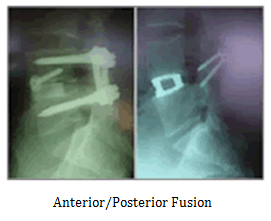 In this operation, the disc is removed by approaching the front of the spine (through the abdomen). In place of the disc is inserted a ring of bone (usually thigh bone) from the bone bank. This is then held at the front with a screw. On occasions, a metal cage made of titanium may be used instead of bone bank bone. Because this insert in the disc space is a relatively weak construction, screws and rods are also required at the back of the spine to hold the implants in place while the bone heals into its new environment.
In this operation, the disc is removed by approaching the front of the spine (through the abdomen). In place of the disc is inserted a ring of bone (usually thigh bone) from the bone bank. This is then held at the front with a screw. On occasions, a metal cage made of titanium may be used instead of bone bank bone. Because this insert in the disc space is a relatively weak construction, screws and rods are also required at the back of the spine to hold the implants in place while the bone heals into its new environment.
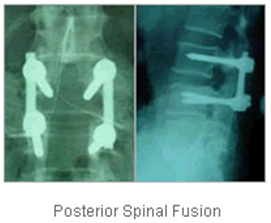
Posterior Fusion
For situations where there is no clear advantage to removing the intervertebral disc, a fusion may be achieved by joining the bones together from behind only. This would usually also involve metal screws and rods.
Posterior Interbody Fusion
It is possible to fuse two back bones across a disc space by placement of a special cage made of carbon fibre from the back of the spine without surgery through the abdomen (TLIF). This surgery may be employed to provide a weight bearing strut from between two adjacent bones and particularly to allow free passage of individual nerves out of the narrowed apertures at the site of the spine where the nerves may be "pinched".
Indications
Spinal fusion may be recommended for:
- Abnormal curvature of the spine: (scoliosis or kyphosis)
- Injury to the spinal vertebrae
- Protrusion of the cushioning disc between vertebrae (slipped disc),
- Weak or unstable spine caused by infections or tumours
What to expect
The outcome from this surgery is usually very successful today with the many available techniques and instruments. The key to a successful outcome is careful choice of which particular patients' conditions are likely to improve with operations.
Convalescence
The patient will be hospitalised for around 6 days after surgery. The repaired spine should be kept in proper position (alignment).
The patient will be taught how to move properly, how to reposition, sit, stand and walk. While in bed, turn frequently using a "log-rolling" technique, meaning that the entire body is moved as a unit, not twisting the spine.
To reduce pain after surgery, an epidural tube is placed in the operative site at the time of surgery, so that a constant flow of pain killing medication can be delivered to the surgical site for the first 2 days after the operation.
The patient will probably have a urinary catheter. Because of the risk of temporary decreased or absent intestinal function (paralytic ileus) after spinal surgery, the patient may not be able to eat for two or so days and will be gradually fed thereafter.
The patient will usually be discharged with a back corset and the family will be taught how to care for this at home.
