 DISC HERNIATION OR HERNIATED NUCLEAS PULPOSUS (slipped disc) -
DISC HERNIATION OR HERNIATED NUCLEAS PULPOSUS (slipped disc) -
A condition in which part or all of the soft, gelatinous central portion of an intervertebral disc (the nucleus pulposus) is forced through a weakened part of its retaining ring, resulting in back pain and possible nerve root irritation.
Usually herniation takes place in the lumbar area of the spine. Lumbar disc herniation occurs 15 times more often than cervical (neck) disc herniation, and it is one of the most common causes of lower back and leg pain. The cervical discs are affected 8% of the time and upper to mid back (thoracic) discs only 1-2% of the time.
Nerve roots (large nerves that branch out from the spinal cord) may become compressed resulting in symptoms such as pain or changes to muscle power or skin sensation. Abnormal function of a nerve from the neck or back is known as “radiculopathy”.
Disc herniation occurs more frequently in middle aged and older men, especially those involved in strenuous physical activity. Other risk factors include any congenital conditions that affect the size of the lumbar spinal canal. Pain or loss of sensation or weakness in the leg which results from a herniation of disc material may give rise to different findings depending on a number of factors including the size of the disc prolapse and the degree to which the spinal nerve is compressed by it.
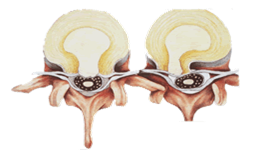
Protrusion vs Extrusion vs Extravasation
A disc protrusion occurs when the material of the nucleus pulposus extends into the retaining ring of the disc without actually rupturing through it. A lump of this material is still able to compress the nerve however and symptoms in the back or leg may result.
A disc extrusion occurs when the material of the nucleus pulposus ruptures through the retaining ring entirely so that this material is situated in the spinal canal adjacent to a nerve root.
A disc prolapse is often larger than the previous varieties and may cause a greater degree of nerve compression.
An extravasation of this material occurs when the gel of the nucleus pulposus has extruded into the spinal canal and formed a free structure which no longer has contact with the retaining ring of the disc. On occasions the extent of nerve compression is not only limited to the single nerve passing to the leg.
When there is a very large amount of nucleus pulposus within the spinal canal all of the spinal nerves may be compressed, particularly those involved in bowel or bladder function, and this is known as Cauda Equina Syndrome. This is usually associated with numbness around the region of the genitals and anus as well as difficulty in passing urine or in bowel movement. This is a serious condition requiring urgent management and any symptoms such as these should be urgently reported to your doctor.
Symptoms of Herniated Lumbar Disc
The most common symptom of a herniated disc is sciatica, a sharp, “shooting” pain that extends from the buttocks down the back of one leg. This is caused by pressure on a spinal nerve often due to a herniated disc. Other symptoms which may be related to sciatica include:
- Weakness in one leg
- Tingling (a “pins and needles” sensation) or numbness in a part of one leg
- Loss of bladder or bowel control (if you also have weakness in both legs, you could have a serious problem. Seek immediate attention)
- A burning pain centred on one side of the back
Other symptoms of a herniated lumbar disc include:
- Severe low back pain, often to one side
- Pain made worse with coughing, straining or laughing
- Muscle weakness or atrophy in later stages
- Muscle spasm causing the trunk to lean to one side
Herniated discs occur most frequently in the lumbar spine – between the bottom of the ribs and your hips – and are most common in people in their 30s and 40s.
Symptoms of Herniated Cervical Disc
Symptoms of a herniated cervical disc include:
- Neck pain, especially in the back and sides of the neck
- Deep pain near or over the shoulder blades on the affected side
- Pain radiating to the shoulder, upper arm, forearm and, rarely, the hand, fingers or chest
- Pain made worse with coughing straining or laughing
- Increased pain when bending the neck or turning the head to one side
- Spasm of the neck muscles
- Altered sensation in the head or arm
- Weakness in one or more muscle groups of one arm
Signs and Tests
A physical examination and history of pain may be sufficient to diagnose the disorder. A neurological examination will be performed to evaluate tendon reflexes, sensation and muscle strength. Often examination of the spine will reveal a decrease in the spinal curvature in the affected area.
Straight leg raising tests that reveals leg pain is diagnostic of a herniated lumbar disc.
A “foraminal compression test of Spurling” will be performed to diagnose cervical radiculopathy. This is performed by bending the head forward and to the sides while downward pressure is applied to the top of the head. Increased pain or numbness during this test is usually indicative of cervical radiculopathy.
Diagnosing a herniated disc
Your medical history is key to a proper diagnosis. You may have a history of back pain with gradually increasing leg pain. Often a specific injury causes a disc to herniate. A physical examination can usually determine which nerve roots are affected (and how seriously). A simple x-ray may show evidence of disc degenerative spine changes.
Diagnostic tests:
- A spine x-ray may be performed to rule out other causes of back or neck pain. However it is not possible to diagnose herniated disc by spinal x-ray alone.
- A spine MRI scan and/or CT scan will show spinal canal compression by the herniated disc.
- A myelogram may be performed to define the size and location of the disc herniation, particularly when a spinal curve is seen. Under normal circumstances, myelography has been superseded by MRI.
Treatment options
Conservative treatment usually works. Most back pain will resolve gradually with simple measures. Bed rest and over the counter pain relievers may be all that is needed. Muscle relaxers, analgesics and anti-inflammatory medications are also helpful. You can also apply cold compresses or ice for no more than 20 minutes at a time, several times a day. After any spasms settle, you can switch to gentle heat applications.
Learning safe work and play practices, proper lifting techniques and weight control may help to prevent back injury in some people.
Most people with leg pain from a pinched nerve due to disc prolapse recover without further intervention within six weeks (about 80%). When pain persists beyond this period, or no improvement is occurring, future treatment may be discussed.
